Dallas Metro / North Texas
(214) 710-1028
August 2022
What is Morton's Neuroma?
Morton’s neuroma, (also referred to as Morton’s metatarsalgia, Morton’s neuralgia, plantar neuroma or intermetatarsal neuroma) is a condition that is caused when the tissue around one of the nerves between your toes begins to thicken. This thickening can result in pain in the ball of the foot. Fortunately, the condition itself is not cancerous.
Morton’s neuroma affects women more often than men with a ratio of 4:1. It tends to target women between the age of 50 and 60, but it can occur in people of all ages. There are some risk factors that may put you at a slightly higher risk of developing the condition. People who often wear narrow or high-heeled shoes are often found to be linked to Morton’s neuroma. Additionally, activities such as running or jogging can put an enormous amount of pressure on the ligament and cause the nerve to thicken.
There usually aren’t any outward symptoms of this condition. A person who has Morton’s neuroma may feel as if they are standing on a pebble in their shoe. They may also feel a tingling or numbness in the toes as well as a burning pain in the ball of their foot that may radiate to their toes.
In order to properly diagnose you, the doctor will press on your foot to feel for a mass or tender spot. He may also do a series of tests such as x-rays, an ultrasound, or an MRI. X-rays are usually done to rule out any other causes for your foot pain such as a stress fracture. Ultrasounds are used to reveal soft tissue abnormalities that may exist, such as neuromas. Your podiatrist may want to use an MRI in order to visualize your soft tissues.
There are three main options for treatment of Morton’s neuroma: Injections, decompression surgery, and removal of the nerve. Injections of steroids into the painful area have been proven to help those with Morton’s neuroma. Decompression surgery has been shown to relieve pressure on the affected nerve by cutting nearby structures such as the ligaments in the foot. Another treatment option would be to surgically remove the growth to provide pain relief.
If you suspect that you have Morton’s neuroma you should make an appointment with your podiatrist right away. You shouldn’t ignore any foot pain that lasts longer than a few days, especially if the pain does not improve.
Pain From Morton’s Neuroma
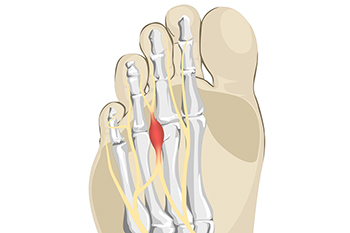
A Morton’s neuroma refers to thickening of nerve tissue at the base of the 3rd or 4th toe. While the precise cause of this condition is unknown, it is thought to form from pressure, irritation, or injury of nerves leading to the toes. This condition can cause one to feel like there is a lump or knot near the ball of the foot, like they are walking on a pebble, or wearing socks that have become bunched up. There can be an achy, sharp, or burning pain in the ball of the foot, or tingling, numbness, or cramping in the forefoot or toes. A Morton’s neuroma can become swollen and painful. One can develop a Morton’s neuroma from wearing shoes that are too narrow where the toes are squeezed together or high-heeled shoes where the body weight is forced onto the ball of the foot. Non-invasive treatments for Morton’s neuroma include wearing properly fitted shoes, with heels less than two inches in height, wide toe boxes, and thick soles, using padding in shoes to take the pressure off the nerve, or taping the feet to redistribute body weight and ease inflammation. Medication and injections can also help relieve pain and pressure of this ailment. Custom orthotics can be made to provide support if one has an abnormal foot structure, such as flat feet or overlapping toes causing the condition. Surgery can be performed if a Morton’s neuroma becomes large or fails to be relieved with more conservative treatment options. Left untreated, a Morton’s neuroma can become worse. For this reason, it is suggested that you visit a podiatrist for a proper diagnosis and treatment that fits the severity of your specific foot problem.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Kellvan Cheng, DPM of Elite Foot & Ankle. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Carrollton, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Cuboid Syndrome
Cuboid syndrome mostly affects athletes, although it can affect non-athletes too. It is also known as cuboid subluxation or cuboid fault syndrome. This condition occurs when joints and ligaments near the cuboid bone of the foot are damaged, or when the cuboid bone itself is dislodged from its natural position. It is usually marked by pain on the outer side of the foot, which may be persistent or may come and go. Cuboid syndrome can be difficult to diagnose unless it becomes severe and more noticeable. Your doctor will likely ask questions about when the pain began and how long it has been present, and will put pressure on the cuboid bone to determine if that area is the origin of the pain.
Causes of Cuboid Syndrome
- Any repetitive stresses placed on the foot due to athletic activities are a common cause of cuboid syndrome.
- Although it develops over time, it is possible that this syndrome can occur all of sudden due to a single event or injury.
- Over-pronation can exacerbate the condition if not corrected.
Disagreements Amongst Podiatrists Regarding Cuboid Syndrome
- Some refer to it as the dislocation of the calcaneal-cuboid joint only.
- Other podiatrists see it as an injury of the ligaments located nearby, which also involves the cuboid bone.
It is very important that when you experience any kind of pain on the side of your foot, you should seek medical care right away. If a subluxed cuboid is caught early, your feet may respond well to the treatment, and you can get back into sports or other activities again as soon as the pain subsides.
Several Reasons Why Cuboid Syndrome May Develop

People who experience pain on the outside of the foot may have cuboid syndrome. This foot condition can follow an ankle sprain and may be difficult to diagnose. It can be common among ballet dancers and can result due to the style of dance they perform. The cuboid bone is one of seven tarsal bones and lies beneath the fourth and fifth toes. If this becomes moved from gradual overuse or an injury, it may become inflamed, referred to as cuboid syndrome. Additional causes of developing cuboid syndrome can include training on uneven surfaces, lack of adequate support from wearing the wrong shoes, or possibly excessive pronation. Some people have intermittent pain and there can be tenderness along the outside of the foot which may be similar to having an ankle injury. There are various treatment options for this condition and it is strongly advised that you are under the care of a podiatrist who can determine the best course of treatment for you.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with Kellvan Cheng, DPM from Elite Foot & Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
- Injury – The most common cause of this ailment is an ankle sprain.
- Repetitive Strain – Tension placed through the peroneus longus muscle from repetitive activities such as jumping and running may cause excessive traction on the bone causing it to sublux.
- Altered Foot Biomechanics – Most people suffering from cuboid subluxation have flat feet.
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact our office located in Carrollton, TX . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes, Symptoms, and Treatment of Poor Blood Circulation in the Feet
Poor blood circulation in the feet and legs is often caused by peripheral artery disease (PAD), which is usually the result of a buildup of plaque in the arteries. Plaque buildup, or atherosclerosis, can be the result of excess calcium and cholesterol in the bloodstream. This restricts how much blood can flow through arteries. Reduced blood flow to a certain area of the body severely limits the amount of oxygen and nutrients that part of the body receives. This leads to degeneration in the muscles and other tissues. Sometimes, poor blood circulation in the feet and legs can be caused by other conditions, such as the damaging or inflammation of blood vessels, known as vasculitis.
The lack of oxygen and nutrients caused by poor blood circulation can restrict muscle growth and development, as well as cause muscle pain and cramps, weakness, and stiffness. Other common symptoms include numbness in the legs and feet, skin discoloration in the affected limbs, slower nail and hair growth, and erectile dysfunction in men. In more severe cases of PAD, pain can be present even when a person isn't exercising, and may range from mildly uncomfortable to completely debilitating.
Poor blood circulation in the feet and legs is more common in those who are overweight or obese, have diabetes, high blood pressure, high cholesterol, who smoke, or who have a family history of PAD or related conditions such as a heart attack, stroke, etc. Diabetes and smoking place a person at greatest risk for developing poor blood circulation, although advanced age, over 50, can also increase risk.
If you are experiencing poor blood circulation in the feet and legs caused by PAD, it is important to make changes to your lifestyle in order to reduce your risk of experiencing a heart attack or stroke caused by this condition. If you smoke, quit completely. This will increase the amount of oxygen in your bloodstream. Exercising and reducing the saturated fats in your diet. Saturated fats come from fatty meats, fried foods, whole milk, etc., can make a difference in improving blood circulation in feet. It is also important to avoid developing influenza and to carefully control your blood sugar if you have diabetes.
Your doctor may recommend combining lifestyle changes with a prescription medication regimen to improve blood circulation. The most commonly-used medications for PAD are called statins and work by blocking the amount of enzymes in your body that produce cholesterol. They are known by the brand names Zocor, Lipitor, Crestor, and others.
Causes and Remedies of Poor Foot Circulation

One of the symptoms of poor circulation is having cold feet. Additional symptoms include swelling, chronic pain, difficulty moving the feet. Many people feel a tingling or numbing sensation in their feet, which may make their feet feel heavy. The common reasons poor circulation may be prevalent among seniors include having diabetes, being overweight, smoking, and living a sedentary lifestyle. There also may be existing medical conditions that contribute to having poor circulation. Among them are having peripheral artery disease (PAD), atherosclerosis, or a venous insufficiency. Circulation can be improved by making lifestyle changes. It is beneficial to incorporate a simple exercise routine daily, and it is important to consume a healthy diet. Some patients find relief when they elevate their feet, and it may help to wear compression stockings. If you would like more information about the causes and remedies of poor circulation in the feet, please confer with a podiatrist.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact Kellvan Cheng, DPM of Elite Foot & Ankle. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our office located in Carrollton, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Do to Keep Your Child’s Feet Healthy
Being a parent involves caring for your child in every way you can. You make sure they are eating the right food, being nice to others, and staying out of any trouble. However, it is also important that you are watchful of their health, more specifically their foot health. Maintaining good foot health in childhood is important in preventing later conditions in life from happening. As children continue to develop, their feet require different techniques of care. Here are some various ways in which you can help your child’s feet stay healthy.
A baby needs a lot of care and attention overall, but the importance of their feet should never be forgotten. Before a baby turns one, their feet change and develop greatly. It is important that during this time, a mother avoids putting tight socks on their child. She should also encourage movement of their feet so the baby can begin to feel more comfortable using them.
As a baby enters the toddler years of his or her life, they are begin to walk around. When your baby begins to take those first steps, it is crucial that they are wearing protective shoes on their feet. As a mother that is observant of your child’s feet, you may notice changes in them. This is completely normal as the feet are becoming susceptible to the activity of walking. It is normal for a toddler to be a bit unsteady or to “walk funny” at first.
When your child grows out of their toddler years, it is important that you begin to show him or her how to care for their feet on their own. Practice with your child proper hygiene in order to prevent foot fungus or infection. Since children are constantly on the move, it is crucial to be cautious of any accidents or injuries that might occur. If an injury occurs, it is advised that you take your child to be examined by a doctor immediately. Since your child is still growing, particular injuries can shift the way in which a bone or other important part of the foot is developing.
Babies and kids are always changing and growing. Your job as a parent is to make sure they stay healthy and making sure they are properly maintained. This involves proper foot care and making sure the feet stay healthy. Following this guide, your child can live a long and happy life.
Odorous Feet in Children

Although having smelly feet is not always necessarily cause for serious concern, bad-smelling feet can be bothersome. If your child is complaining about their feet producing a foul odor, there are several things that you need to be aware of. The odor that is being emitted from your child’s feet is caused by bacteria. After your child spends a whole day sweating in a pair of sneakers, for instance, that sweat facilitates the multiplication of bacteria. If your child is not wearing socks, typically this only exacerbates the extent to which the bacteria can grow in your child’s shoes. In certain cases, your child’s shoes might even be home to a type of bacteria named Kyetococcus sedentarius. This bacteria can produce especially foul odors because they release volatile sulfur compounds. If you are concerned about your child’s smelly feet, be sure that they wash their feet and wear a new, clean pair of socks every day and alternate shoes regularly, especially if they get wet or sweaty. See a podiatrist for more ways in which you can protect the health of your child’s feet.
Making sure that your children maintain good foot health is very important as they grow. If you have any questions, contact Kellvan Cheng, DPM of Elite Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
Keeping Children's Feet Healthy
Having healthy feet during childhood can help prevent medical problems later in life, namely in the back and legs. As children grow, their feet require different types of care. Here are some things to consider...
Although babies do not walk yet, it is still very important to take care of their feet.
Avoid putting tight shoes or socks on his or her feet.
Allow the baby to stretch and kick his or her feet to feel comfortable.
As a toddler, kids are now on the move and begin to develop differently. At this age, toddlers are getting a feel for walking, so don’t be alarmed if your toddler is unsteady or ‘walks funny’.
As your child gets older, it is important to teach them how to take care of their feet.
Show them proper hygiene to prevent infections such as fungus.
Be watchful for any pain or injury.
Have all injuries checked by a doctor as soon as possible.
Comfortable, protective shoes should always be worn, especially at play.
If you have any questions please feel free to contact our office located in Carrollton, TX . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Keep Your Feet Healthy So You Can Stay Active
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
Blog Archives
- July 2025
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017